Direct and indirect pulp capping using Bio-C Repair bioceramic cement
BIO-C® Repair | Angelus
Isabela Arieta Carula, specialist in Endodontics
Clauber Romagnoli, specialist in Endodontics and Implantology; Master in Endodontics
Douglas Giordani Negreiros Cortez, specialist in Endodontics and Implantology; Master and PhD in Endodontics
Renato Interliche, specialist in Endodontics and Implantology; Master in Endodontics
Abstract
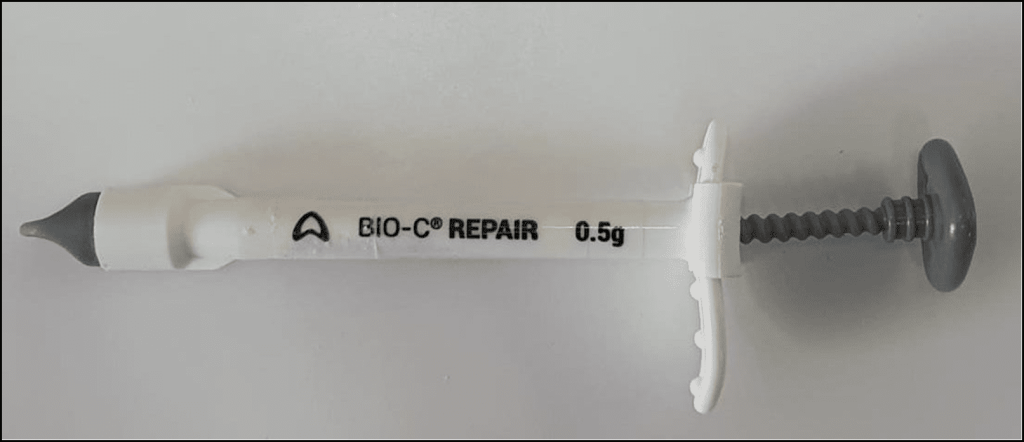
This study aimed to report two clinical cases of direct pulp capping using a bioceramic cement (Bio C Repair Angelus, Londrina, PR, Brazil). Two patients were selected at the specialization clinic of the Escola Educação Inteligente (EI-UNINGÁ, Londrina, PR, Brazil) who had extensive and unsatisfactory composite resin restorations, and who, during removal, pulpal exposure occurred. Proservation and radiographic follow-up of the cases were performed 30 and 60 days after the procedure. One patient did not return to the clinic and the second patient did not report any symptoms during the period. Direct pulp protection is performed when dental pulp is exposed during cavity preparation and aims to reduce injuries and promote tissue healing. Bioceramic was developed to improve the properties of MTA (Mineral Trioxide Aggregate) and currently, one of its indications is direct pulp protection. This material has properties such as biocompatibility, bioactivity, hydrophilicity, dimensional stability, short setting time, absence of toxicity, bactericidal action due to the alkaline pH, and easy handling since it does not require handling. Due to these properties, the success rate using bioceramics is high in the endodontic area.
Keywords: Direct pulp capping. Mineral trioxide aggregate. Bioceramics in Endodontics.
Introduction
Dental caries is a multifactorial, infectious, transmissible, and diet-dependent disease that causes demineralization of dental structures forming a cavity. The interaction of factors: microorganisms, diet, time, and susceptible tooth define the concept of caries (Lima, 2007). It consists of an intermittent process that can evolve through repeated phases of remission and recurrence and can result in the complete destruction of the affected tooth when the disease is not treated (Thylstrup, 1990).
The objective of contemporary Endodontics is to preserve pulpal vitality, enabling complete root development, preventing apical periodontitis, and presenting minimally invasive therapies seeking to maintain the maximum of healthy tooth structure.
In cases where the caries reach the dentin, it is possible to detect by means of the interproximal radiograph a zone of hard dentin between caries and the pulp. In extremely deep caries, where the entire extension of the dentin is reached, pulp exposure is inevitable during treatment. Teeth that had the pulp exposed during excavation should not necessarily undergo root canal treatment. However, when:
1) carious exposure causes symptoms of irreversible pulpitis; 2) when absolute isolation is not being used; 3) the field is not aseptic; 4) the instruments used are contaminated during the removal of carious tissue, the tooth must undergo pulpectomy.
Maintaining tooth vitality is important to conserve pulpal defense mechanisms and allow dentin formation. However, it is necessary evaluate some factors such as patient age, exposure size, remaining tooth structure, results of thermal and percussion tests, and pulp diagnosis. Healthy pulp with an uncompromised blood supply at the time of capping is essential for vital pulp treatment to be successful (Awadeh et al. 2018).
Pulp capping is a procedure where the exposed pulp is covered by a protective material, minimizing injuries and allowing the tissue to heal (Queiroz et al. 2005). The objective of this procedure is to keep the largest number of viable cells to react to the carious process. These new cells (odontoblasts) are derived from undifferentiated mesenchymal cells and form reactional dentin (Guedes et al. 2006). Although calcium hydroxide (Ca(OH)2) is the most used material for this purpose, studies carried out with MTA show that this biomaterial provides a lower inflammatory response, the dentin bridge formation is thicker and more uniform with less tissue necrosis (Catalá et al. 2008). Ca(OH)2 when compared to MTA, shows incomplete dentin bridge formation with defects that can lead to failure of direct pulpal protection (Liu et al. 2015)..
A study conducted by Accorinteet al. (2008) aimed to evaluate dental pulps histomorphologically capped with MTA and calcium hydroxide showed that in the group of teeth capped with MTA, pulp healing was faster than that of Ca(OH) cement.2. However, both groups responded well to capping and both cements are excellent for capping human teeth.
Mineral Trioxide Aggregate – MTA was the first bioceramic introduced in Endodontics by Torabinejad in 1993. The bioceramic is composed of tricalcium and dicalcium silicates, calcium phosphate, calcium hydroxide, and zinc oxide as a radiopacifier, alumina, and bioactive glass (Lima et al 2007).
With the evolution of this material, several studies were carried out so that bioceramics could be used in more procedures, mainly in the field of endodontics, such as, for example, in sealing perforations, pulp capping, retrograde filling, and apexification of teeth with incomplete rhizogenesis (Raghavendra et al. al. 2017). Therefore, we can describe the characteristics of this material in such a way that it explains why its use by dentists is increasing. It has tissue biocompatibility (Torabinejad et al. 2010), minimizing tissue inflammation, enabling cell proliferation on the material, and inducing the differentiation of undifferentiated pulp cells to form odontoblasts. It has a high pH value (Zhang et al. 2009) which confers antimicrobial capacity; it is radiopaque, hydrophilic, insoluble, and has low cytotoxicity (Jingzh et al. 2011). Stimulates the formation of mineralized tissue similar to hydroxyapatite composition from the new odontoblastic cells that have been formed (Lucio, 2007). Thus, the objective of this study was to report two clinical cases where there was pulp exposure during cavity preparation and the treatment instituted was direct pulp capping with bioceramic Bio-C Repair (Angelus, Londrina, BR).
Case Report
Clincal Case 1:
A female patient, 23 years old, asymptomatic, attended the clinic of the Specialization course in Endodontics at the Educação Inteligente school (Ei Uningá, Londrina- Paraná, Brazil) for evaluation of element 47.
The pulp vitality was confirmed through the thermal test. During the clinical examination, the presence of extensive restoration in composite resin was verified and confirmed in the radiographic examination, which also allowed to demonstrate the proximity of the lesion to the pulp chamber, as shown in figure 1.

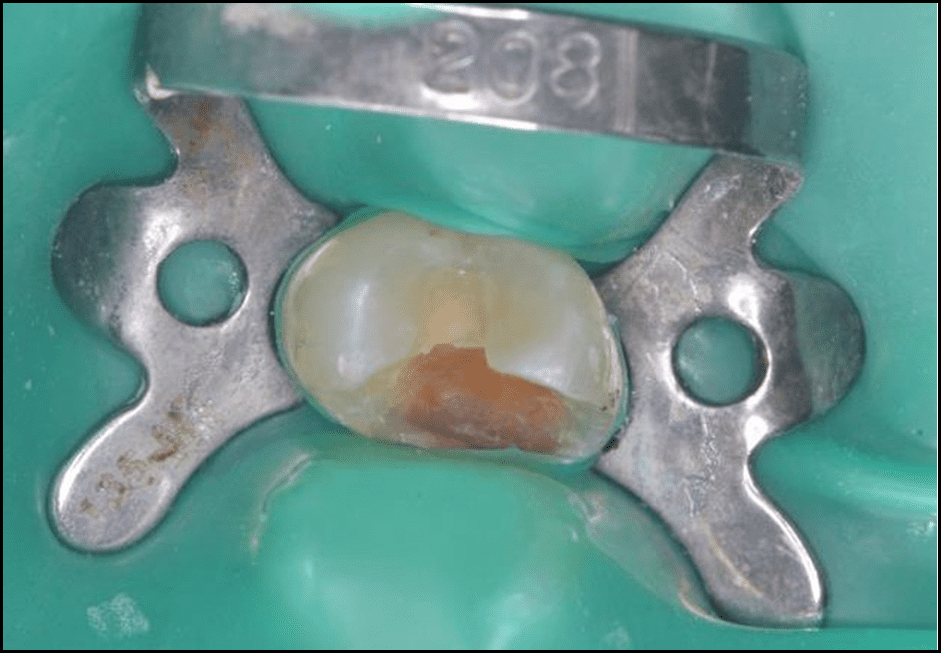
The patient was anesthetized, absolute isolation was performed and the element was sealed with a gingival barrier. To remove the restoration and the decayed tissue, a high-speed spherical diamond bur and a spherical drill bit were used low rotation, taking into account the risk of pulpal exposure. During excavation, the pulp was exposed (figure 2 and 3).


Homeostasis was performed with a cotton ball soaked in saline solution. After controlling the bleeding, direct pulp capping was then performed with Bio C Repair bioceramic cement (Angelus, Londrina, BR) (Figures 4 to 6). The restoration of the cavity was made with composite resin. A new periapical radiograph was taken to verify the material in the cavity (Figure 7).



Data regarding postoperative pain, state of sensitivity, radiographic signs of periapical pathology and dentin bridge formation were analyzed.
The patient was instructed to return to the clinic in 30 days for follow-up of the case and follow-up of the element with new radiographs and clinical examination, however, she did not attend the return visit.
Clinical Case 2:
Male patient, 37 years old, asymptomatic, attended the clinic of the postgraduate course Educação Inteligente – Ei Uningá (Londrina- Paraná, Brazil) for evaluation of element 15, which had extensive and unsatisfactory restoration in composite resin (Figure 8).

Through the thermal test, pulp vitality was verified. The composite resin restoration was removed with diamond burs at high speed, the decayed dentin removed manually with a curette and with the aid of a spherical drill at low speed. After the field was duly isolated with a rubber dam, hemostasis was performed with saline solution, Bioceramic Bio-C Repair was used as a capping material for the pulp, and the tooth was restored with composite resin (Figures 9 and 10).


Evaluation after 30 days for clinical and radiographic control (figure 12) and follow-up of the element. The patient reported no symptoms.

Discussion
In 1993, Torabinejad introduced MTA in dental practice and, since then, this material has undergone several evolutions and improvements. Bioceramics include aluminum and zirconia, bioactive glass, calcium silicates, calcium phosphates, and hydroxyapatite in their composition (Oliveira, 2014).
The choice of bioceramics as a capping material was based on articles that prove the success of living pulp treatments using this material.
A study evaluated the biocompatibility of MTA after direct pulp capping in dog teeth, and the result shows that after 90 days it had formed a thick, compact dentin bridge and completely obliterated the pulp exposure. There was no presence of inflammation, the pulp tissue was normal, with fibroblasts, and a moderate amount of collagen was observed (Queiroz et al. 2005).
Success is due to the properties of bioceramics, such as biocompatibility, providing less tissue irritation, ability to induce dentin bridge formation, easy handling, low cytotoxicity, and antimicrobial effect due to the high pH that remains constant after the setting reaction.
Bioceramics are more biocompatible, they are hydrophilic, and dimensionally more stable, it is also considered a bioactive material, that is, it is capable of interacting with living tissues, resulting in the formation of an apatite layer at the material-tissue interface during the hardening process. With the studies that have been carried out around this new material, the predictability of the treatment of live pulps can be defined.
The study of Linu et al. (2017), which compares the effect of MTA and Biodentine on teeth that underwent direct pulp protection, shows a success rate of 84.6% and 92.3% respectively. In addition, in relation to the formation of a dentin bridge, they obtained a similar result between the two groups (69.2% and 61.5%). Moreover, for these authors, the success of living pulp therapy can be considered from the formation of an impermeable barrier involving the pulp tissue that was exposed.
Dental pulp has a potential for natural tissue repair, that is, it manages to form repairing dentin. This ability generates a hard tissue barrier (dentin bridge) after performing direct pulp capping. The original odontoblasts at the site of exposure are destroyed and replaced by differentiated odontoblast-like cells.
In vitro studies demonstrated that MTA has the ability to stimulate cell differentiation, which contributes to the formation of the hard tissue matrix. There is a limited necrosis of the pulp tissue after its application, however, the material most used to perform direct pulp capping is calcium hydroxide (Ca (OH)2) it is the least caustic of this reaction, as calcium hydroxide causes the formation of a necrotic layer along the material-pulp interface, in addition to inducing the formation of repairing dentin in a greater proportion and with better structural integrity (Okijiet al. 2009).
Conclusion
Within the limitations of this study, we can conclude that bioceramic cements are a viable and promising alternative for direct pulpal protection, with further studies still to be carried out to confirm these results.
References
Accorinte MLR, Holland R, Reis A, Bortoluzzi MC, Murata SS, Dezan Jr E, et al. Evaluation of Mineral Trioxide Aggregate and Calcium Hydroxide Cement As Pulp-Capping Agents In Human Teeth. Journal Of Endodontics. V. 34, N. 1, p. 1-6. 2008.
Awawdeh L, Al-Qudah A, Hamouri A, Chakra RJ. Outcomes of Vital Pulp Therapy Using Mineral Trioxide Aggregate or Biodentine: A Prospective Randomized Clinical Trial. Journal Of Endodontics. V. 44, N.11, p. 1603-1609. 2018.
Catalá CJT, Gonzalez CM, Bernal DG, Sanchez REO, Forner L, et al. Biocompatibility of New Pulp-capping Materials NeoMTA Plus, MTA Repair HP, and Biodentine on Human Dental Pulp Stem Cells. Journal Of Endodontics. V.44, N.1, p.126-132. 2018.
Duncan HF , Galler KM , Tompson PL , Simon S , El-Karin I , Rundzina R , et al. European Society of Endodontics position statement: Management of Deep Caries and the Exposed Pulp. International Endodontic Journal. V.52, N.7, p.923–934. 2009.
Guedes CC, Santos EM, Fernandes KPS, Martins MD, Bussadori SK. Direct Pulp Capping in a Young Permanent First Molar Using Mineral Trioxide Aggregate (MTA).Rev. Inst. Science Health.V.24, N.4, p.331-335. 2006.
Jingzhi M, Shen Y, Stojicic S, Haapasalo M. Biocompatibility of Two Novel Root Repair Materials. Journal Of Endodontic. V.37, N.6, p.793- 798. 2011.
Lima J.E.O. Dental caries: a new concept.Rev. Dental Press Ortodon Ortoped Facial. V.12, N.6, p.119-130. 2007.
Lima NFF, Dos Santos PRN, Pedrosa MS, Delboni MG. Bioceramic cements in endodontics: literature review.Rev. of the Faculty of Dentistry.V.22, N.2, p.248-254. 2017.
Linu S, Lekshmi MS, Varunkumar VS, Sam Joseph VG. Treatment Outcome Following Direct Pulp Capping Using Bioceramic Materials in Mature Permanent Teeth with Carious Exposure: A Pilot Retrospective Study. Journal Of Endodontics. V.43, N.10, p.1635-1639. 2017.
Liu S, Wang S, Dong Y, Dong Y. Evaluation of a Bioceramic as a Pulp Capping Agent In Vitro and In Vivo. Journal Of Endodontics. V.41, N.5, p.652-657. 2015.
Lucio D. Mineral Trioxide Aggregate (MTA) Direct Pulp Capping: 10 Years Clinical Results. Italian Journal of Endodontics.V.31, N.1, p.48-57. 2017.
Okiji T, Yoshiba K. Reparative Dentinogenesis Induced by Mineral Trioxide Aggregate: A Review from the Biological and Physicochemical Points of View. International Journal Of Dentistry. September. 2009.
Oliveira PS. Bioceramics in Endodontics. [Thesis]. Porto, Portugal:Fernando Pessoa University Faculty of Health Sciences. 2014.
Queiroz AM, Assed S, Leonardo MR, Filho NP, Silva LAB. MTA And Hydroxide For Pulp Capping. Appl Oral Sci. V.13, N.2, p.126-30. 2005.
Raghavendra SS, Jadhav GR, Gathani KM, Kotadia P. Bioceramics in Endodontics – A Review.. Journal Istanbul Univ Fac Dent. N.51, p.128-2017.
Thylstrup A. Clinical Evidence of the Role of Pre-eruptive Fluoride in Caries Prevention. Journal Dent Res. V.69, N.2, p.742-750. 1990.
Torabinejad M, Parirokh M. Mineral Trioxide Aggregate: A Comprehensive Literature Review-Part II. Journal Of Endodontics. V.36, N.2, p.190-202. 2010.
Zhang H, Shen Y, Ruse ND, Haapasalo M. Antibacterial Activity of Endodontic Sealers By Modified Direct Contact Test Against Enterococcus Faecalis. Journal Of Endodontics. V.35, N.7, p.1051- 1055. 2009.
Produtos em destaque
 Materiais Informativos
Materiais Informativos
Acesse bula, catálogo, perfil técnico e trilhas de conhecimento para saber mais sobre nossos produtos!
Leia também
Nenhum caso clínico encontrado 😅
We use cookies to provide you with a better experience, improve performance, analyze how you interact on our website and customize content. By using this website, you agree to the use of cookies.
OK, I GOT ITWe use cookies to provide you with a better experience, improve performance, analyze how you interact on our website and customize content. By using this website, you agree to the use of cookies.

SAC
Specialized Customer Service
Monday to Friday, from 7:30 a.m to 5:30 p.m (GMT-3).



2 comentários
07/04/2024
How does the effectiveness of Bio-C Repair bioceramic cement compare to traditional materials in direct and indirect pulp capping techniques, as discussed in the article?Visit us Telkom University
17/04/2024
Hello! We have sent your question to the responsible department, don’t forget to keep an eye on your spam folder